Environmental
What are Environmental Pulmonary Fibrosis and Hypersensitivity Pneumonitis?
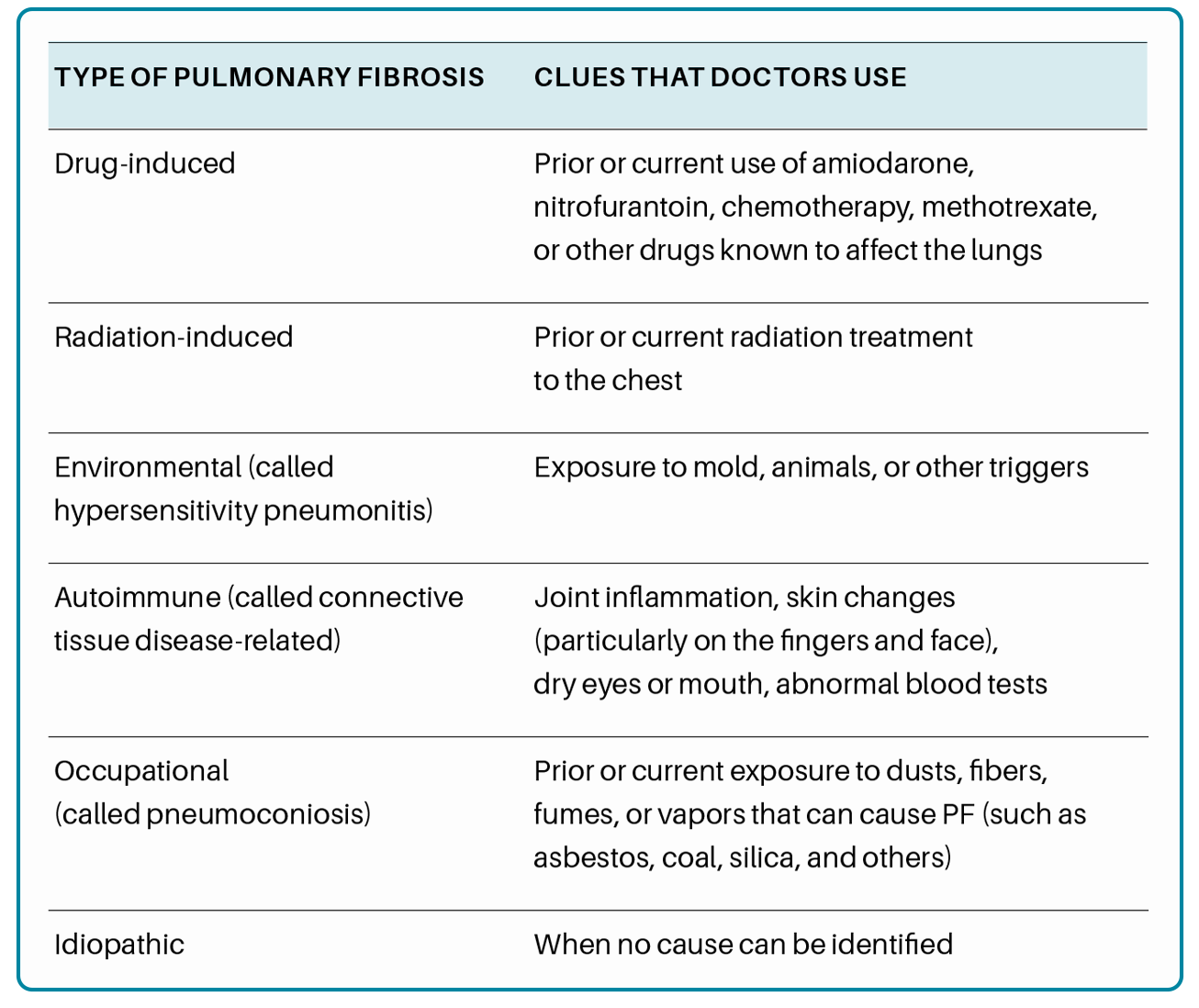
Pulmonary fibrosis (PF) is part of a larger group of more than 200
interstitial lung diseases (also known as ILDs) that are characterized by inflammation and/or scarring in the lung. In ILDs, the injury and damage occurs in the walls of the air sacs of the lung, as well as in the tissue and space around these air
sacs. When an interstitial lung disease includes scar tissue in the lung, we call it pulmonary fibrosis.
One of the subgroups of interstitial lung disease is those that are related to environmental exposures, referred to as “hypersensitivity pneumonitis. ” Hypersensitivity pneumonitis (HP) results from the lungs’ reaction to inhaled organic particles or “antigens”. This reaction can involve inflammation or scarring (also known as fibrosis), or a combination of both.
- This type of lung injury can be acute, in which case the problem is usually more inflammatory and can be reversible with avoidance of the exposure causing the disease.
- HP can also have a more subtle onset, “subacute” or “chronic” form, which can have a less dramatic presentation. In these cases, there is more fibrosis or scarring injury to the lungs, which is not fully reversible.
What are the Symptoms of Hypersensitivity Pneumonitis?
Shortness of breath and cough are the most common symptoms in patients with HP. Tightness of the chest, wheezing, weight loss, chills, and body aches can also occur. Symptoms can come and go and may be more severe when spending time in a particular location, such as a vacation or primary home, or the workplace. Some people experience symptoms that develop suddenly over days to weeks, and others have subtle symptoms that slowly worsen over years. Fatigue, depression, and anxiety are also commonly experienced by people living with HP.

How is Hypersensitivity Pneumonitis Diagnosed?
When a doctor or other healthcare provider suspects that a patient has ILD, they will collect information about the patient’s medical and personal history, work and home environment, hobbies, and illness that may be present in the family. This can help a doctor identify exposures or other diseases that might have caused lung injury and scarring. The doctor will also often order pulmonary function tests, a chest x-ray, blood work, and a high-resolution CT scan.
Pulmonary function tests measure how much air the lungs can hold, and how the lungs are working overall. Scarring can cause the lungs to shrink, and it can also make them stiff and unable to fully expand. This means the lungs are able to hold less air. Scar tissue may also affect the ability of the lungs to transfer oxygen to the bloodstream.
Blood work (serology) can provide information about exposures that may have caused a person’s lung injury, or show that other diseases are present which may be associated with the development of PF.
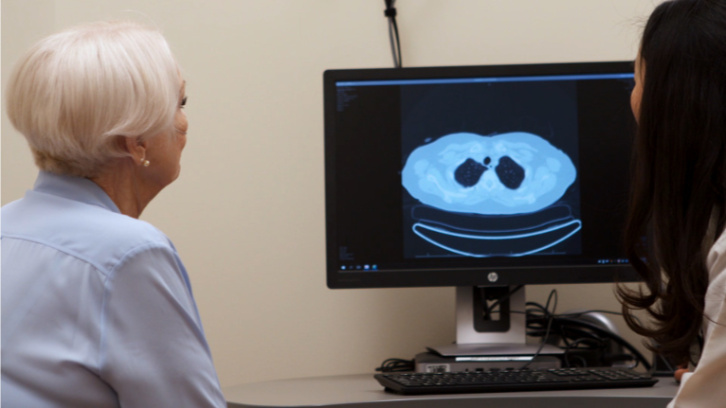
A high-resolution computed tomography (HRCT) scan is a special type of x-ray that shows fine detail of the lung tissue. On a CT scan (also known as CAT scan) healthy lung tissue looks nearly black, and scar tissue and inflammation appear grey or white.
When a doctor or other healthcare provider suspects that a patient has HP, they will discuss with you potential “antigen” (inhaled particle) exposures in the environments that you frequently visit. Unfortunately, even with a complete history, not all patients can identify the trigger for their disease. In some cases, a bronchoscopy or lung biopsy may be performed to aid in diagnosis but cannot typically help to identify a specific exposure.
What are the Causes of Hypersensitivity Pneumonitis?
HP is the result of a reaction to inhaling particles or “antigens” in the air. Some of the “antigens” that may cause HP include airborne mold, airborne dusts from birds or feathers, hot tub use, and humidifier use. In some cases, the antigen cannot be identified. On the other hand, some people never become ill despite exposure to antigens known to cause HP. Genetic differences might explain why this occurs.

How is Hypersensitivity Pneumonitis Treated?
If a specific antigen exposure can be identified, avoiding or removing it from the environment is an important part of HP treatment. Sometimes medications that suppress the immune system are used to try to halt the damage being done to the lungs and to reverse inflammation if it is present. For patients who have progressive fibrosis (worsening scarring) as part of their disease, their pulmonologist might consider the use of an anti-fibrotic medication to slow the scarring.
Supplemental oxygen, pulmonary rehabilitation, and management of symptoms are important treatment options for many types of pulmonary fibrosis, depending on how severe the disease is. Lung transplantation may also be considered for some patients. Smoking cessation and routine vaccinations are important parts of living with pulmonary fibrosis. Additional research is ongoing to determine the best approach to treat this type of interstitial lung disease.
What Should I Do Next?
If you have been recently diagnosed with pulmonary fibrosis, consider making an appointment with a pulmonologist who has experience caring for patients with PF. A knowledgeable team of experts will help make sure you receive an accurate diagnosis and
the most up-to-date treatments and management recommendations. To assist you in finding pulmonologists nearest to your home who provide expert care to patients with PF, the Pulmonary Fibrosis Foundation established the PFF Care Center Network, which includes 74 medical centers throughout the United States. You can search for the PFF Care Center Network medical center closest to
you here.
We also recommend that you join a pulmonary fibrosis support group. Connecting with other individuals facing the same illness can help you and your family feel less alone in your journey with pulmonary fibrosis. Support groups can supplement the care
you receive from your healthcare team by providing emotional support and education. You can find a list of support groups here.
Support groups can help those living with pulmonary fibrosis to:
- Learn about their disease and available treatments
- Feel supported by others who share similar experiences living with PF
- Learn to navigate the healthcare system more effectively
- Improve coping skills, connect with helpful resources, and more
Contact the PFF Help Center by calling 844.TalkPFF (844.825.5733) or email help@pulmonaryfibrosis.org. We can help answer your questions, discuss your concerns, and connect you with resources.