Other Types of Pulmonary Fibrosis
Other Types of Pulmonary Fibrosis
Pulmonary fibrosis (PF) is part of a larger group of more than 200 interstitial lung diseases (also known as ILDs) that are characterized by inflammation and/or scarring in the lung. In ILDs, the injury and damage occurs in the walls of the air sacs of the lung, as well as in the tissue and space around these air sacs. When an interstitial lung disease includes scar tissue in the lung, we call it pulmonary fibrosis.
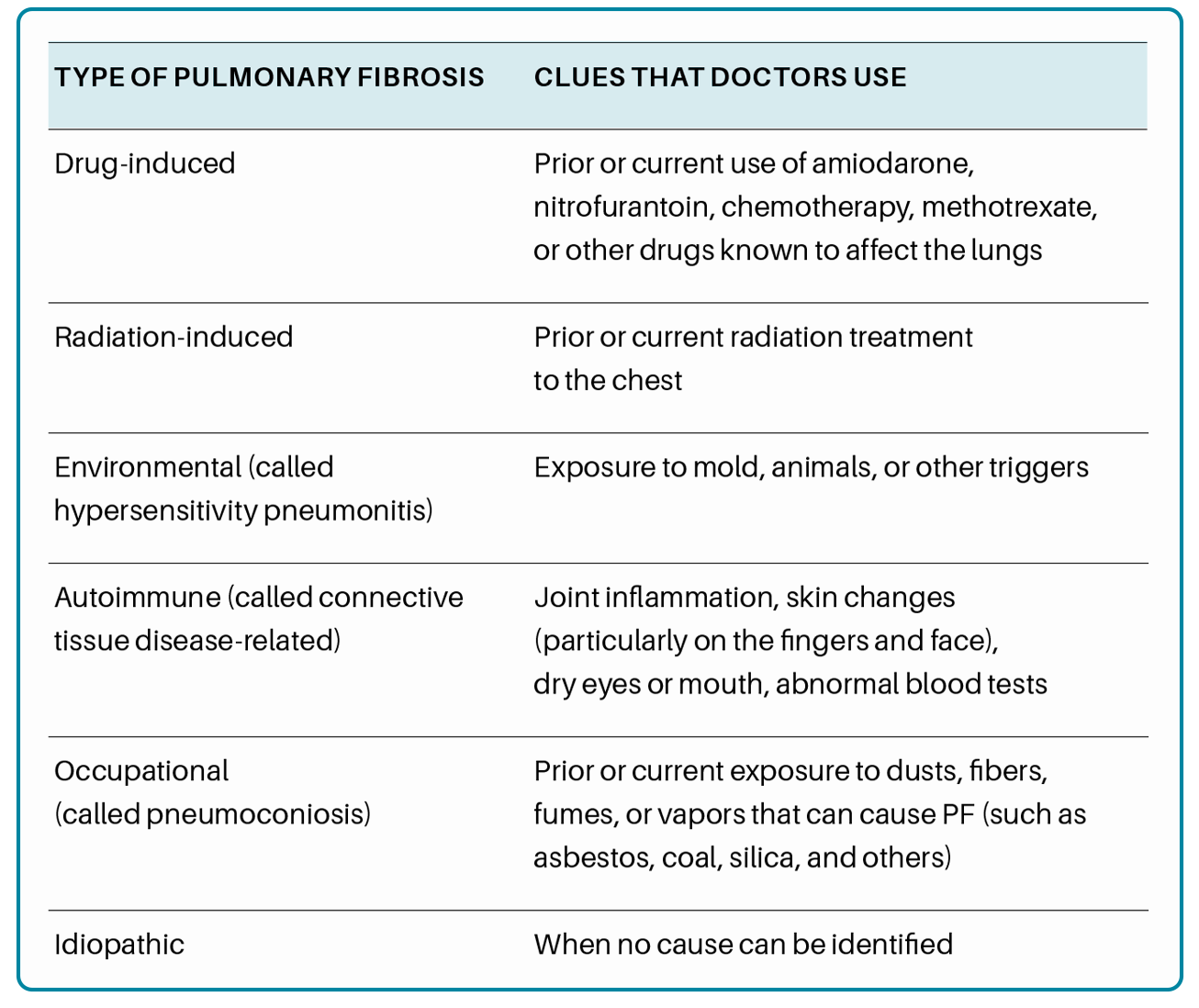
There are types of pulmonary fibrosis that do not fall into the categories of environmental, occupational, drug-induced, radiation-induced, connective tissue disease-related, or idiopathic interstitial lung disease. Some forms of ILD are caused by another condition, like sarcoidosis or lymphangioleiomyomatosis, or may be the after-effect of acute respiratory distress syndrome, which occurs in critical illness. Other forms of pulmonary fibrosis may have a genetic component, like familial pulmonary fibrosis and pulmonary fibrosis associated with Hermansky Pudlak syndrome or dyskeratosis congenita. Some patients have forms of pulmonary fibrosis that do not fit into any of the known categories of interstitial lung disease or have overlapping features of multiple types of ILD, which is termed “unclassifiable interstitial lung disease (ILD)”.
Pulmonary Fibrosis Associated with Sarcoidosis
Sarcoidosis is an inflammatory disease of unknown cause, in which granulomas (clumps of inflammatory cells) form in one or more organs in the body. Early symptoms of sarcoidosis can include a skin rash, swollen or painful joints, fever, or enlarged lymph nodes. Symptoms of advanced sarcoidosis can include fatigue, irregular heartbeat, visual problems, weakness or numbness in the limbs or parts of the face, and unexplained weight loss. Disease characteristics and severity of sarcoidosis can vary greatly from patient to patient.
While it can affect any organ in the body, the lungs are affected in 90% of patients with sarcoidosis. While spontaneous remission occurs in a majority of sarcoidosis cases, chronic inflammation in the lungs can lead to pulmonary fibrosis. Once scar tissue is present in the lungs, it cannot be reversed.
Supplemental oxygen, pulmonary rehabilitation, and management of symptoms are important treatment options for many types of pulmonary fibrosis, depending on how severe the disease is. Smoking cessation and routine vaccinations are important parts of living with pulmonary fibrosis. Treatments specific to sarcoidosis-associated pulmonary fibrosis can include medications like corticosteroids and immunosuppressants.


Pulmonary Fibrosis Following Acute Respiratory Distress Syndrome (ARDS)
When a person experiences acute and severe injury to the lung, they may develop acute respiratory distress syndrome (ARDS) which causes inflammatory fluid to enter the air sacs in the lung. ARDS can result in respiratory failure and the need for mechanical ventilation. Causes of ARDS can include infection (such as sepsis, influenza, or pneumonia), trauma, burn injuries, or breathing in high concentrations of smoke or other fumes, resulting in damage to the air sacs in the lung.
As the lungs heal from these overwhelming injuries, patients can develop post-ARDS fibroproliferation or “fibrosis”. Post-ARDS fibrosis and pulmonary fibrosis that occurs in other types of interstitial lung disease (ILD) have distinct differences. While many other types of ILD are chronic and progressive in nature, post-ARDS fibrosis typically is not progressive, but nonetheless can be severe and limiting. The recovery period for post-ARDS fibrosis can take as long as one year and the remaining deficits to lung function persist, but generally do not progress.
Supplemental oxygen, pulmonary rehabilitation, and management of symptoms are important treatment options for many types of pulmonary fibrosis, depending on how severe the disease is. Smoking cessation and routine vaccinations are important parts of living with pulmonary fibrosis.
Pulmonary Fibrosis Associated with Lymphangioleiomyomatosis (LAM)
Lymphangioleiomyomatosis (LAM) is a rare disease that affects multiple organ systems in the body and is found almost exclusively in women. In LAM, smooth muscle cells grow at an abnormal rate, particularly in the lungs, kidneys, and lymphatic system. Those affected by LAM are grouped into two categories: sporadic LAM, which occurs for unknown reasons; and LAM caused by tuberous sclerosis complex (TSC), a rare disease. Uncontrolled growth of smooth muscle cells in lung tissue due to LAM can block airways and release fluid into the lungs that can result in cystic lung damage.
While there currently is no cure for lung disease associated with LAM, there are medications (sirolimus and everolimus) that may improve lung function in some patients living with LAM. Supplemental oxygen, pulmonary rehabilitation, and management of symptoms are important treatment options for many types of pulmonary fibrosis, depending on how severe the disease is. Smoking cessation and routine vaccinations are important parts of living with pulmonary fibrosis. Lung transplantation may be an option for some patients with LAM-associated pulmonary fibrosis.


Familial Pulmonary Fibrosis
A diagnosis of familial pulmonary fibrosis (FPF) should be suspected when a PF patient has at least one other closely related family member affected by pulmonary fibrosis. These patients should be considered for genetic counseling and testing. Currently, it is estimated that up to 20% of people with pulmonary fibrosis have familial pulmonary fibrosis (FPF).
We are still learning about all the possible causes of FPF. It is important to know that there is not simply one gene or one variant that causes FPF. Inherited gene variants in two important pathways are known to be related to FPF. The more frequent variants are in genes that are related to protecting the telomeres. Telomeres are specialized structures located at the ends of chromosomes that serve to protect our chromosomes throughout our lifetime.
- Variants in several telomere regulatory genes (TERT, TERC, PARN, DKC1, NAF1, RTEL1, ZCCHC8, and TINF2) have been discovered and account for 20-30% of FPF cases.
- Variants in genes of another pathway, the surfactant genes (SFTPA1, SFTPA2, SFTPC, ABCA3 and NKX2-1) are less common and account for 1-3% of familial cases.
There are also rare genetic conditions where pulmonary fibrosis can be a secondary feature, such as pulmonary fibrosis associated with Hermansky Pudlak syndrome and dyskeratosis congenita. In patients with idiopathic pulmonary fibrosis (IPF) who do not have a family history of PF, cases of telomerase gene variants have been reported in approximately 1-5% of patients. However, common variants in multiple genes have been associated with development of PF. Common variants are defined as being present in 5-10% of healthy individuals, but are found more frequently in patients with IPF. While these variants can also be passed down in families, they are thought to have less impact on the development of IPF compared to the rare variants in the genes listed previously.
Patients with FPF or likely inherited forms of pulmonary fibrosis should be seen for a genetic evaluation and counseling to determine what, if any genetic testing is appropriate and to educate the patient about risks and benefits of genetic testing.
Unclassifiable Interstitial Lung Disease
“Interstitial lung disease” refers to a large group of respiratory diseases that cause inflammation and / or scarring in the lung tissue, or “interstitium”. When an ILD includes scar tissue in the lung, we call it pulmonary fibrosis. Some patients with interstitial lung disease do not fall into a specific category of pulmonary fibrosis, even with multidisciplinary discussion among expert pulmonologists, radiologists, and pathologists. A patient may be diagnosed with “unclassifiable interstitial lung disease” if they do not meet all the criteria to be confidently diagnosed with a specific type of interstitial lung disease or pulmonary fibrosis. This occurs when there are nonspecific or conflicting findings on their CT scans, lung biopsies, or in the clinical course of the disease. Another case when a diagnosis of unclassifiable ILD may occur is when the patient is unable to go through standard diagnostic tests.
Supplemental oxygen, pulmonary rehabilitation, and management of symptoms are important treatment options for many types of pulmonary fibrosis, depending on how severe the disease is. Lung transplant may be an option for some patients with unclassifiable ILD. Smoking cessation and routine vaccinations are important parts of living with pulmonary fibrosis.


What Should I Do Next?
If you have been recently diagnosed with pulmonary fibrosis, consider making an appointment with a pulmonologist who has experience caring for patients with PF. A knowledgeable team of experts will help make sure you receive an accurate diagnosis and
the most up-to-date treatments and management recommendations. To assist you in finding pulmonologists nearest to your home who provide expert care to patients with PF, the Pulmonary Fibrosis Foundation established the PFF Care Center Network, which includes 68 medical centers throughout the United States. You can search for the PFF Care Center Network medical center closest to
you here.
We also recommend that you join a pulmonary fibrosis support group. Connecting with other individuals facing the same illness can help you and your family feel less alone in your journey with pulmonary fibrosis. Support groups can supplement the care
you receive from your healthcare team by providing emotional support and education. You can find a list of support groups
here.
Support groups can help those living with pulmonary fibrosis to:
- Learn about their disease and available treatments
- Feel supported by others who share similar experiences living with PF
- Learn to navigate the healthcare system more effectively
- Improve coping skills, connect with helpful resources, and more
Contact the PFF Help Center by calling 844.TalkPFF (844.825.5733) or email help@pulmonaryfibrosis.org. We can help answer your questions, discuss your concerns, and connect you with resources.
Acknowledgments
Foundation for Sarcoidosis Research
Janet Talbert, MS, CGC, LGC | Vanderbilt University Medical Center
References:
Ryerson CJ, Urbania TH, et. al. Prevalence and prognosis of unclassifiable interstitial lung disease. European Respiratory Journal. Sep 2013; 42 (3): 750-757.
Schwarz MI, King TE. Interstitial Lung Disease. Fifth Edition. Shelton, CT: People’s Medical Publishing House-USA; 2011. 472-578 p, 1061-1073 p.
Educational Materials
Find reliable information and trusted resources that can help you learn about pulmonary fibrosis and live better with PF.
-
View Full Details
Pulmonary Fibrosis Information Guide
Our comprehensive guide provides reliable information about pulmonary fibrosis, the diagnostic process, treatment options, and more. -
View Full Details
Genetic Testing for You and Your Family
This position statement provides guidance on familial pulmonary fibrosis and key information to consider prior to genetic counseling.

PFF Help Center
For those living with pulmonary fibrosis, obtaining the most accurate and current information can be a frustrating and challenging task. Let us help you find your answers.