Rural Outreach in Pulmonary Fibrosis: Patient Statement
What is Pulmonary Fibrosis?
The word “pulmonary” means lung and the word “fibrosis” means scar tissue— similar to scars that form on the skin from an old injury or surgery. Pulmonary fibrosis (PF) is a process that causes lung scarring, in which fibrotic tissue blocks the movement of oxygen from inside the tiny air sacs in the lungs into the bloodstream. Low oxygen levels (and the stiff scar tissue itself) can cause people who have pulmonary fibrosis to feel short of breath, particularly when walking and exercising.
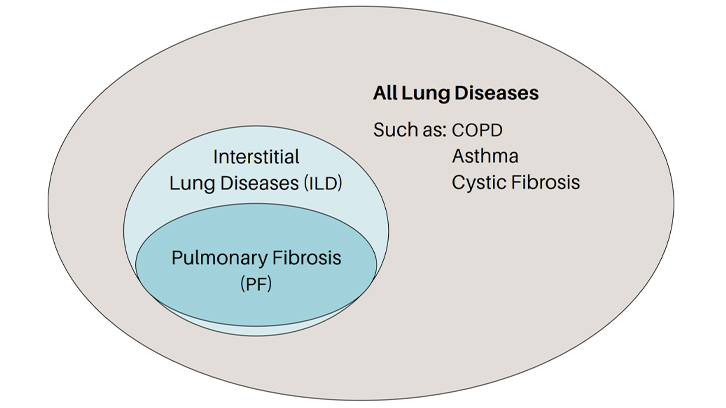
Pulmonary fibrosis isn’t just one disease. It is a family of more than 200 different lung diseases that all look very much alike. The PF family of lung diseases is part of an even larger group of diseases called interstitial lung diseases (also known as ILD), which includes all of the diseases that have inflammation and/or lung scarring. In ILDs, it is the walls of the air sacs of the lung, and the tissue and space around these air sacs, where the injury and damage occur. Some interstitial lung diseases don’t include lung scarring. When an interstitial lung disease does include scar tissue in the lung, we call it pulmonary fibrosis.
Resources for Patients Living with Pulmonary Fibrosis in Rural Areas
Telemedicine
Telemedicine
definition: Telemedicine is the use of technology (smartphone, tablet,
laptop, or desktop computer) that enables patients to communicate
directly with members of their healthcare team. Benefits of telemedicine
include access to specialists not located close to a patient’s home.
Televisits between patients and healthcare providers can be conducted by
video or phone. Preparation by the patient is the most important
prerequisite for a successful televisit. You can be more prepared by
referring to the resources below.
Resources
- Telemedicine
Basics for the Pulmonary Fibrosis Patient Booklet
- Checklist
for a Successful Telemedicine Visit
- Telemedicine 101: Making the Most of Your Virtual Visits Video
Support Groups
Connecting
with others facing similar experiences can improve emotional well-being
and have a positive impact on the health of people who are living with
pulmonary fibrosis. Support groups provide an opportunity for
participants to share experiences, practical information, and resources.
A support group can also be a valuable source of encouragement and
inspiration for patients, caregivers, family members, and friends.
Virtual support groups have more recently emerged and can provide access
to those with electronic devices and by telephone.
The PFF hosts
monthly virtual support groups for anyone who is affected by pulmonary
fibrosis using a program called Zoom. If you are not able to attend an
in-person group, or simply want more opportunities for support between
meetings, consider joining one of the PFF’s monthly support group calls.
To find a support group near you or to learn more about the PFF’s monthly virtual support groups, you can use our interactive map.
Medication
Drug therapy
for pulmonary fibrosis is often specific to each type of PF. Due to
differences in the causes of PF, a medication prescribed to treat one
form of the disease may not be right for another. It is important to
discuss drug therapy with your healthcare provider to learn what
medications may be appropriate to treat your form of pulmonary fibrosis.
PF medications have differing side effects which may be unfamiliar to
many clinicians outside of medical centers with expertise in caring for
patients with PF. Shared decision-making is improved by a knowledge of
anticipated side effects and is important in helping patients to make
the right choice for them. Many times, staying on these medications
requires some lifestyle/diet changes, dose changes or even taking
over-the-counter or prescription medication to keep going.
Monitoring
side effects and lab studies is an essential component of the safe use
of medications. There is also collaboration between the prescribing
provider and the local healthcare provider regarding blood testing,
tracking results, and sharing those results with the patient.
Resources
- Fact sheets on a variety of medications
- PFF YouTube playlist Treatment and Symptom Management
- Information on the PFF Care Center Network
Pulmonary rehabilitation
Pulmonary rehabilitation (PR) is a structured exercise program designed for people living with chronic lung diseases like pulmonary fibrosis (PF). Exercise can give you more energy and improve your focus, your mood, and your overall sense of well-being.
Pulmonary rehabilitation includes:
- Exercise training
- Education on managing your disease
- Learning how to develop behavior change strategies and stick with healthy behaviors
In-person PR is at this time considered the most effective and safest model of PR in the US. However, some people aren’t able to attend an in-person pulmonary rehabilitation (PR) program because of distance or cost. The PFF has developed a Pulmonary Rehabilitation Toolkit that provides some of the information and resources that you would receive through a pulmonary rehabilitation program, although these are not a substitute for in-person pulmonary rehabilitation (see resources below). Talk with your health care provider before starting any new exercise routine, including those found online, to make sure that it is safe and appropriate for you
Resources
- Pulmonary Rehabilitation Toolkit, including exercise videos
- AACVPR Pulmonary Rehabilitation Program Directory
Oxygen Therapy
People
living with lung disease often have lower than normal levels of oxygen
in their blood. When oxygen saturation levels drop to 88% or lower, a
healthcare provider may order supplemental oxygen. Oxygen is not
addictive and does not weaken your lungs. Use it as prescribed by your
healthcare provider.
The benefits of oxygen therapy may include:
- Reducing breathlessness
- Increasing your ability to maintain an active lifestyle
- Helping to reduce stress on other organs
Patients
may experience difficulty accessing supplemental oxygen. This may be
especially true in rural areas, when the durable medical equipment (DME)
companies (these are companies that provide oxygen and equipment) may
be located far from rural patients. If you have questions about your
oxygen equipment, get in touch with the DME company that serves your
community.
Resources for Oxygen Therapy
Palliative Care
Palliative
care is specialized care for people living with any serious illness
that causes a high burden of symptoms such as pulmonary fibrosis.
Palliative care focuses on providing relief from the symptoms and stress
that pulmonary fibrosis can cause. The goal is to improve your and your
caregiver’s ability to enjoy life. A palliative care team usually
consists of trained doctors, nurses, social workers, and other team
members who work together with your existing care team to provide an
extra layer of support.
Resources
- Palliative Care Position Statement
- Symptom Management for PF: How Palliative Care Can Improve Quality of Life
- Getpalliativecare.org
Lung transplantation
Lung
transplantation may be an option for some patients with pulmonary
fibrosis. The Scientific Registry of Transplant Recipients (SRTR) lists
74 centers in the United States that perform lung transplantation, and
these centers are predominantly located in urban areas. This means that
patients living in rural areas likely have to travel greater distances
to be evaluated at a lung transplantation center. Lung transplant
criteria and evaluations varies by center and your healthcare provider
can help you understand if this is an option you may need to consider.
Resources
- Preparing
for a Lung Transplant Booklet
- Life
After Lung Transplant Booklet
- Lung Transplant Playlist on YouTube
Clinical Trials
Clinical trials for pulmonary fibrosis treatment are research studies that explore whether a medical strategy, treatment, or device is safe and effective for humans. These studies also may show which medical approaches work best for certain illnesses or groups of people. Clinical trials for pulmonary fibrosis treatment produce the best data available for health care decision making.
The purpose of clinical trials is
research, so the studies follow strict scientific and ethical standards.
These standards protect patients and help produce reliable study
results.
Patients with pulmonary fibrosis may find several advantages
to joining a clinical trial. Participants may obtain access to a
potential new PF medication and receive valuable education about
improving their health. Increased clinic visits and testing usually
associated with a clinical trial may give the participant a clearer
picture of the state of their disease and progression. Many PF clinical
trial participants say that even if joining a trial doesn’t directly
benefit them, they view it as an important step on the road to helping
future patients with PF.
Clinical trials are more likely to be available at academic medical centers in urban areas. Patients living outside of urban areas may need to travel farther to participate in clinical trials. Trial sponsors may consider providing financial support for travel or other accommodations for patients living outside of urban areas. Some clinical trials are done primarily online and may also be an option.
Rural Health Outreach Committee
Tejaswini Kulkarni, MD; University of Alabama - CHAIR
Rebecca Bascom, MD, MPH; Penn State - CHAIR
Alison DeDent, MD; University of California San Francisco
Christopher King, MD; Inova Fairfax
Hyun Kim, MD; University of Minnesota
Mark Hamblin, MD, FCCP; University of Kansas
Janell Reichuber, APRN; University of Kansas
Jennifer Wescoe; Wescoe Foundation for Pulmonary Fibrosis
Divya Patel, MD; University of Florida
Franck Rahaghi, MD, MHS, FCCP; Pulmonary Fibrosis Foundation, Cleveland Clinic Florida
Ryan Boente, MD; Indiana University
Zeenat Safdar, MD; Houston Methodist
Anoop Nambiar, MD; UT Health Science Center at San Antonio
Amy Case, MD; Piedmont Healthcare, Pulmonary Fibrosis Foundation
Mary Beth Scholand, MD; University of Utah
Sonye Danoff, MD, PhD; Johns Hopkins, Pulmonary Fibrosis Foundation
Amy Gietzen; Patient Representative
Jim Carns; Patient Representative
Richard Bell; Patient Representative
Jessica Shore, PhD, RN; Pulmonary Fibrosis Foundation
Kate Gates; Pulmonary Fibrosis Foundation
Laura Devitt; Pulmonary Fibrosis Foundation
Ingrid Schwab; Pulmonary Fibrosis Foundation
Aubrey Trecek; Pulmonary Fibrosis Foundation