Rural Outreach in Pulmonary Fibrosis: Provider Statement
What is Pulmonary Fibrosis?
The goal of this statement is to increase awareness of pulmonary fibrosis (PF) in rural communities and to describe the Rural Health Initiatives of the Pulmonary Fibrosis Foundation (PFF). We present a framework identifying rural disparities and gaps in the current care of patients living with PF and provide recommendations of the PFF Rural Health Outreach Committee based on our current understanding of the challenges and opportunities. While there is no single definition or measurement of rurality, we identify rurality measures based on geographical proximity to urban areas (nonmetro counties outside the boundaries of metro areas); further subdivided into micropolitan areas (10,000 – 49,000) and non-core counties and those areas with populations ranging from 2,500 to 50,000 (ers.usda.gov).
Are there rural disparities for pulmonary fibrosis?
Recent studies show disparities in rural U.S. patients with idiopathoic pulmonary fibrosis (IPF), including increased risk for IPF, decreased antifibrotic utilization, and worse disease severity at presentation, explained by indicators of worse neighborhood-level socioeconomic status. The PFF Rural Health Outreach Committee supports a multi-pronged research agenda to amplify our understanding of rural disparities in PF.
What do we know about current barriers to clinical care?
Current barriers for clinician referral of their patients to institutions with PF expertise include increased travel time and distance to specialized centers, inefficient provider-to-provider communication, different electronic medical record systems, and limitations in clinical information sharing technologies. Rural communities face health professional shortages, lack of services, decreased access to health insurance, and increased rates of poverty. The cumulative impact of these disparities is increased risk of delayed diagnosis and limited access to specialty providers and comprehensive treatment plans.
What strategies might currently address barriers?
We identify strategies that impact patient care, research, and advocacy.
Remote multidisciplinary conferences assist with diagnostic accuracy and knowledge dissemination
The PFF Rural Health Outreach Committee strongly supports the PFF goal to build capacity and increase access for community pulmonologists to participate in multidisciplinary discussions (MDDs), an evidence-based approach to ILD diagnosis and management. The MDD consists of a facilitated discussion between pulmonologists, thoracic radiologists, pulmonary pathologists, and rheumatologists to arrive at an individualized diagnostic and management consensus. The MDD provides a forum for dissemination of updated diagnostic and treatment guidelines, medication monitoring and side effect management, management of acute exacerbations, and clinical trial availabilities.
For a remote MDD, there needs to be an interactive platform that is accessible to multisite participants. Logistical obstacles include ease of login and a HIPAA-consistent approach to sharing clinical information. Implementation science research is needed to identify additional strategies for conducting virtual MDDs with rural providers that align with variable staffing models, capacity, and schedules.
Synchronous and Asynchronous Telemedicine could improve access to care
The PFF Rural Health Outreach Committee supports the development of high-quality implementation science data for the increasing use of telemedicine for PF care. Current resources from the PFF can be found at https://www.pulmonaryfibrosis.org/patients-caregivers/education-resources/telemedicine. Synchronous telemedicine, with the healthcare provider and patient in direct visual and auditory contact, requires broadband access. PFF Care Centers provide regional telemedicine capabilities. Asynchronous telemedicine, sometimes called “store and forward,” collects clinical information and sends it to another site for review and evaluation. In this model, the specialist has no direct interaction with the patient, but assists with triage, and guides the local practitioner. This approach has more flexibility as the patient, local practitioner, and specialist do not have to be available at the same time. For PF, this might include forwarding a clinical vignette, pulmonary functions studies, laboratory data, and a chest CT scan to a PF specialist or MDD for their review and recommendation. Implementation of asynchronous activities would require that PF specialists and their local health system create appropriate payment relationships and HIPAA compliant communication networks. There is a need for careful evaluation of synchronous and asynchronous telemedicine care models for PF in rural communities.
Care networks facilitate access advanced therapies
Shared decision-making is facilitated by a knowledge of anticipated side effects for the patient through patient education material and co-management between PF specialists and community providers. Specialty pharmacy access may be a potential solution to supporting patient and provider education regarding therapies.
Focuses of current capacity building: pulmonary rehabilitation, oxygen therapy, and community EMS partners
The PFF Rural Health Outreach Committee strongly supports building capacity to have pulmonary rehabilitation (PR) in rural communities (PFF resources) and further investigation on tele-rehab. We also support monitoring oxygen policy to ensure this is equitably distributed to all geographic regions. Supplemental oxygen can relieve dyspnea and anxiety and improve daily physical activity and health-related quality of life. It is recommended that patients being started on oxygen in the rural setting be provided with rural focused education about oxygen therapy, including back-up power systems. EMS providers and associated community paramedicine programs could provide access to supplemental oxygen during natural disasters or other crisis situations where oxygen suppliers may not be able to conduct regular deliveries.
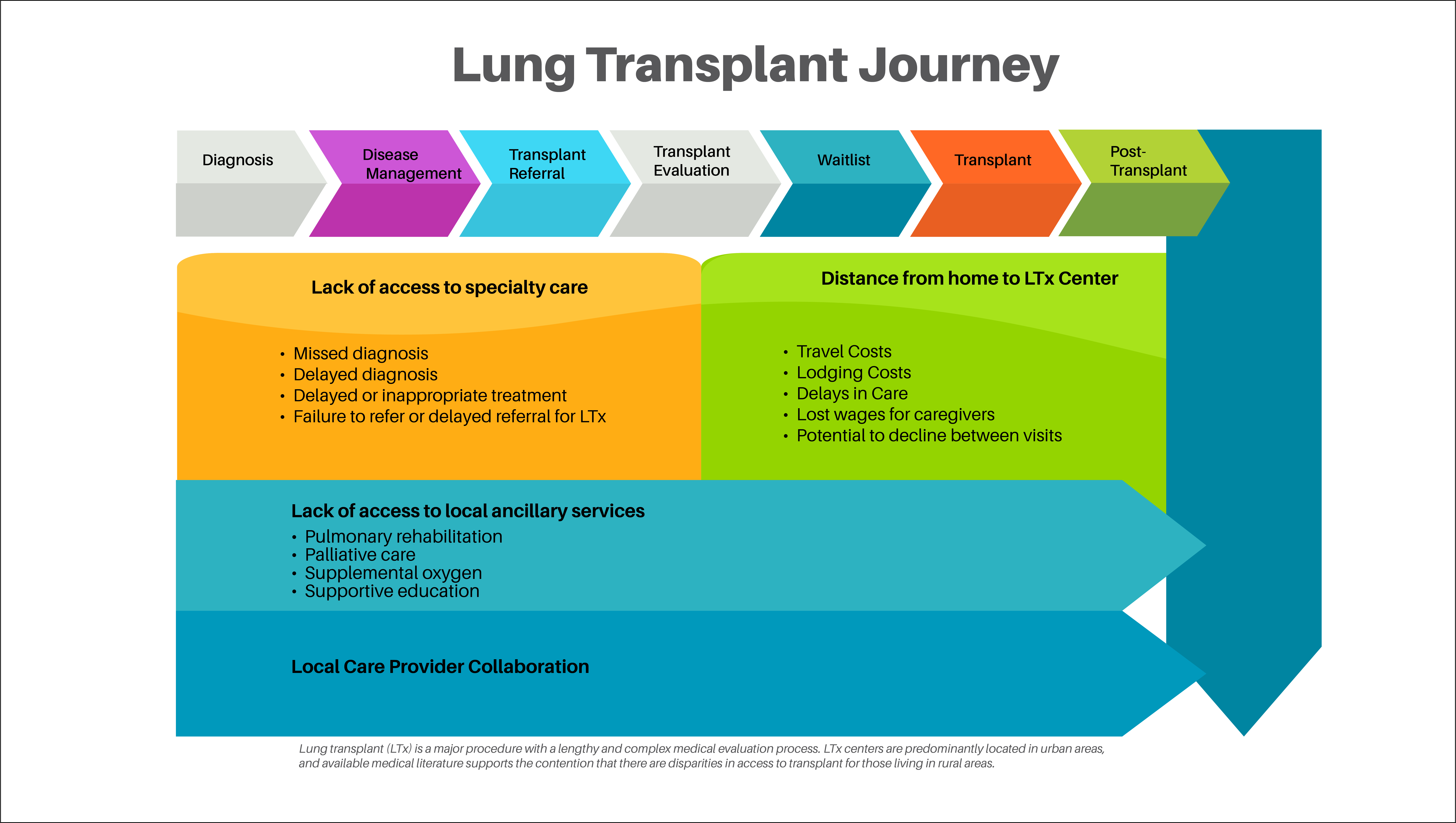
Lung transplantation
The 74 centers in the United States that perform lung transplant are predominantly located in urban areas, and available medical literature supports the contention that there are disparities in access to transplant for those living in rural areas. The existing medical literature only accounts for differences in outcomes for those patients evaluated at transplant centers; Figure 1 shows other sources of potential disparities along the continuum of care.
Click the image to view the full-screen size.
Multipronged approach to increase access to clinical trials
The committee supports the adoption of successful strategies to increase access and participation of rural patients in clinical trials (Figure 2). Clinical trials may offer patients access to emerging treatment options; however, clinical trial sites are highly clustered around urban areas. There are several barriers to rural Americans participating in clinical trials, including lack of knowledge, understanding of specific information about their diagnosis or clinical trials, mistrust of researchers or physicians, and lack of transportation.
Click the image to view the full-screen size.
Networks facilitate accessing local sources of palliative care
Palliative care (PC) can augment the management of patients with life-changing pulmonary fibrosis by addressing symptoms, supporting caregivers, and aiding in end-of-life planning. Access to palliative care in rural areas still lags when compared to more urban areas. Expanding access to PC includes educating providers and patients/caregivers, including those in rural areas. These discussions are further outlined in this PFF position statement.
Conclusion
To summarize, the overarching goal of the PFF is to establish baseline information and benchmarks with which to measure the success of our efforts to improve outcomes for people living with PF in rural communities. This statement provides recommendations of the PFF Rural Health Outreach Committee based on our current understanding of the challenges and opportunities in the management of persons living with PF who reside in rural communities.
Rural Health Outreach Committee
Tejaswini Kulkarni, MD; University of Alabama - CHAIRRebecca Bascom, MD, MPH; Penn State - CHAIR
Alison DeDent, MD; University of California San Francisco
Christopher King, MD; Inova Fairfax
Hyun Kim, MD; University of Minnesota
Mark Hamblin, MD, FCCP; University of Kansas
Janell Reichuber, APRN; University of Kansas
Jennifer Wescoe; Wescoe Foundation for Pulmonary Fibrosis
Divya Patel, MD; University of Florida
Franck Rahaghi, MD, MHS, FCCP; Pulmonary Fibrosis Foundation, Cleveland Clinic Florida
Ryan Boente, MD; Indiana University
Zeenat Safdar, MD; Houston Methodist
Anoop Nambiar, MD; UT Health Science Center at San Antonio
Amy Case, MD; Piedmont Healthcare, Pulmonary Fibrosis Foundation
Mary Beth Scholand, MD; University of Utah
Sonye Danoff, MD, PhD; Johns Hopkins, Pulmonary Fibrosis Foundation
Amy Gietzen; Patient Representative
Jim Carns; Patient Representative
Richard Bell; Patient Representative
Jessica Shore, PhD, RN; Pulmonary Fibrosis Foundation
Kate Gates; Pulmonary Fibrosis Foundation
Laura Devitt; Pulmonary Fibrosis Foundation
Ingrid Schwab; Pulmonary Fibrosis Foundation
Aubrey Trecek; Pulmonary Fibrosis Foundation